July 14, 2013
I am sharing this beautiful video in gratitude. http://www.values.com/inspirational-stories-tv-spots/122-Annie-s-Song
It is fantastic when you enlarge it to full screen size while listening to John Denver’s timeless song.
Talking About Health; Why Health Communication Matters
A BLOG to support my book, Talking About Health; Why Health Communication Matters
July 14, 2013
I am sharing this beautiful video in gratitude. http://www.values.com/inspirational-stories-tv-spots/122-Annie-s-Song
It is fantastic when you enlarge it to full screen size while listening to John Denver’s timeless song.
February 4, 2011
 Aieeeeeeeee. Dr. Oz had some visiting doctors on his show again today. As they were wrapping up some of the discussion, Dr. Oz said, “Genes load the gun… The environment pulls the trigger… I want you to remember that.” What?! We have discussed the importance of family health history in this forum before. So the role of genetics is one that is an important topic when talking about health.
Aieeeeeeeee. Dr. Oz had some visiting doctors on his show again today. As they were wrapping up some of the discussion, Dr. Oz said, “Genes load the gun… The environment pulls the trigger… I want you to remember that.” What?! We have discussed the importance of family health history in this forum before. So the role of genetics is one that is an important topic when talking about health.
But I wonder how many viewers really got the idea that it was family health history they should be thinking about with his expression–“Genes load the gun.” This is an old metaphor for the role of genes for health and has not been very effective. Add to that, the conversation that Dr. Oz was having about genetic mutations on the show. It all got mushed together…
“The environment pulls the trigger.. I want you to remember that.” Really? What does it mean? Again, the meaning of environment in this metaphor has many interpretations. Environment for most people is about where they live, the climate, the neighborhood, pollution… those things all matter when it comes to our health and interact with our family health history. But environment includes our personal behavior and our social environment–friends, family, and culture. What we eat, for example, is part of the ‘environment’ that our genes live in… But I am not confident that this meaning is clear when talking about genes and health with this metaphor…
 Then there was the conversation about viruses–that cause cancer. HPV was one of the two examples discussed. I think that this also was not a good way to discuss the issue. If I have cervical cancer, you cannot ‘catch’ it from me. Cervical cancer is not a virus that can be passed from one woman to another. Cervical cancer is often caused by the lesions that form from genital warts caused by HPV–the humanpapilloma virus. So there is a virus that causes a condition that may be the cause of cancer…and not just cervical cancer but also penile cancer and throat cancer and head and neck cancers… So we may pass a virus between us that leads to genital warts that sometimes do not heal and may cause some changes in our cells and become cancer…
Then there was the conversation about viruses–that cause cancer. HPV was one of the two examples discussed. I think that this also was not a good way to discuss the issue. If I have cervical cancer, you cannot ‘catch’ it from me. Cervical cancer is not a virus that can be passed from one woman to another. Cervical cancer is often caused by the lesions that form from genital warts caused by HPV–the humanpapilloma virus. So there is a virus that causes a condition that may be the cause of cancer…and not just cervical cancer but also penile cancer and throat cancer and head and neck cancers… So we may pass a virus between us that leads to genital warts that sometimes do not heal and may cause some changes in our cells and become cancer…
So let’s focus on understanding that increases our health literacy and not shorthand expressions that don’t… And let’s look toward spring and the daffodils that will replace the frozen icy tundra in my woods today…
December 20, 2010
 Tens of thousands of us develop blood clots each year. Sometimes, they start as a pain in your thigh. Often, the cause is too little movement for too long a period of time. Hence, the need to take breaks and walk around if you are traveling in a car. Get up and move about on the plane or train or bus. Stretch your toes forward from your ankles when you are sitting and then pull your toes back. Repeat half a dozen times.
Tens of thousands of us develop blood clots each year. Sometimes, they start as a pain in your thigh. Often, the cause is too little movement for too long a period of time. Hence, the need to take breaks and walk around if you are traveling in a car. Get up and move about on the plane or train or bus. Stretch your toes forward from your ankles when you are sitting and then pull your toes back. Repeat half a dozen times.
Stay hydrated. Drink water and not alcohol. For more advice about traveling and blood clots, visit http://www.mdtravelhealth.com/illness/deep_vein_thrombosis.html.
AND, talk to your family about this. Ask, “has anyone had a blood clot?” Your family history may predict greater than average risk. All of us need to avoid cramped spaces and long periods of not moving around. Some of us may have a family history that suggests we should be tested for genetic contributors to clotting. You won’t know if you don’t…ask.
August 9, 2010
I attended Bret Michaels concert at the Clearfield, PA county fair on Friday night. 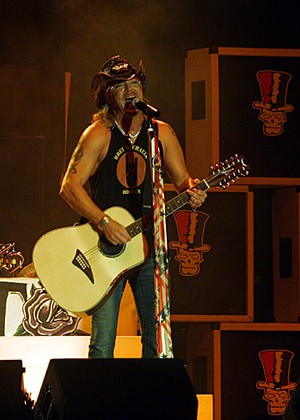 It was a celebration of life. He thanked fans for their prayers and support for him during the past year. He literally seemed to breathe in the positive energy and well wishes of the fans at the concert. Which communicated something about health…. http://gantdaily.com/2010/08/07/bret-michaels-rocks-at-the-clearfield-county-fair/
It was a celebration of life. He thanked fans for their prayers and support for him during the past year. He literally seemed to breathe in the positive energy and well wishes of the fans at the concert. Which communicated something about health…. http://gantdaily.com/2010/08/07/bret-michaels-rocks-at-the-clearfield-county-fair/
As covered in the news and entertainment media, Bret had some life-threatening health events this year. He appeared on the show, ‘Celebrity Apprentice’ and, in fact, won… but during the season, he revealed his nearly lifelong efforts to manage diabetes. And he talked about the emotions he felt while waiting for news about whether his daughter had the disease.
I don’t know Bret or his daughter. But I do know that one of the reasons we don’t talk about health in our families is that we feel a sense of blame for the ‘bad’ things that got passed on to us through our genetic pool and a sense of responsibility about passing them along to our own biological children.
Try this: for every so called bad thing, make a list of the good things that were passed on to us and that we may pass on to others. When having those family health history conversations, balance the good with the not so good news.
It might be, for example, that Bret’s positive and affirming way of looking at life has a genetic component and that he will or has already passed on such resilience to his children. I suspect that at the very least, that attitude goes a long way toward helping him to manage life with a chronic condition like diabetes…
 May 19, 2010
May 19, 2010
Health disparities…differences in the health status of some of us compared to others–have many links to communication. We could place more emphasis on efforts to address some of these as part of health care reform.
One communication contributor to health disparities is a lack of equal access to health information. In particular, a digital divide has been identified as leading to differences in people’s awareness and understanding of ways to promote health and treatments for various diseases.
The digital divide has been discussed for years in terms of the affordability and availability of computers. This contributed to programs to increase access to computers in public schools and public libraries. Access to sources of health information is an important goal–one that may be enhanced by improving the nation’s infrastructure. I was struck by a colleague’s recent revelation on our way to a meeting in a rural community in Pennsylvania. He said that he seldom uses the internet from home. In his location, internet access still depends on the use of a dial-up modem. The slow and painful effort to get online just isn’t worth it. Libraries and schools in his area suffer from the same challenges.
The effort to reduce the digital divide by increasing access to online health resources is a good start but reminds me of the ‘just build it and they will come’ fallacy. Once we get on the computer, and we use our favorite search engines to look for health information, how do we decide whether the information is useful and relates to us? How do we understand the information? How do we harness resources to apply the information when we do understand it? That includes having sites for care and providers for care. …that includes having the ability to pay for care, time off to receive care, and transportation to sites for care.
Health disparities becomes a communication issue with many facets and many audiences to consider. If we approach health disparities as only an issue relating to access to information, we risk placing blame for continuing and/or growing disparities on people experiencing the disparities.
In a world where access to health information was supported by access to services, products, and care–our individual perceptions still may lead to disparities. Understanding related to the information and choices to apply the content depends on some knowledge of health terms and ability to translate the metaphors so often used to commmunicate in health information. Understanding also depends on the cultural and social lens through which we view the information. And on our own goals–including where we place responsibility for health.
Some of us assume more personal responsibility for our health than others. Some of us believe more in the role of family history and genetics than others. Some of us believe that the environment plays a greater role in our health than our own behavior. And some of us believe in a role for spirituality and religious faith. When we combine these into our health perspective, sometimes health disparities emerge… Can erasing a digital divide make a difference in these issues? Perhaps if we communicate about them directly, online and in other settings where we talk about health.
 May 12, 2010
May 12, 2010
Watching my 5 year old granddaughter play youth soccer was great fun. Such energy. Such excitement. Such effort. Everyone running toward the ball and doing their best to get in a good kick. Sometimes in their enthusiasm, they lost sight of which goal they should be aiming for and may even accidentally kick the ball into the other team’s space. It’s a bit like health care reform in the U.S.
Keep ‘health’ in health communication… this is one of my mantras. I remind myself of it when thinking about the value of my own health communication research and the value of work that I review. It reminds me to consider, “how will the work make a difference in the health of someone?” Will it, for example, help someone to make a decision about which treatment to choose, which food to eat, how important rest and fun can be for health? Will it help someone to talk with family members about health history or to disclose to family members, doctors, or others important information about health status? Will it enable others to provide emotional or tangible social support to keep to a health regimen? …and so on.
So when I listen to conversation about health care reform, I am struck by several trends. First, there is so much fear and anger in the discourse. My mom, for example, will be having hip replacement surgery this summer. She is in her late 70s and on Medicare. She is convinced that her doctor will be paid very little for her surgery because of health care reform. She is also fearful that if she doesn’t act now, she may not be able to even find a doctor who will do the surgery soon…because the doctors won’t be paid well and won’t accept patients on Medicare.
We know quite a bit about fear appeals in communication. And sure enough, what I hear suggests to me that for many, the talk about health care reform and the actual reform itself does not make the efficacy of the actions clear. How will this reform be an effective response in both promoting ‘health’ of citizens and in limiting the runaway expenses? How might each one of us feel more confident or gain the ability to make decisions about our own health based on the reform? Made to feel fearful, many become angry and direct it toward the source.
Second, there has been too little direct translation of how health care reform will benefit health. Health illiteracy and science illiteracy often provide a way to explain our lack of understanding about health issues. Health insurance illiteracy is a whole new ball game. Most of us have some experience with car insurance or home owner insurance or life insurance, so we fall back on those as a way to understand health care insurance and health care reform. We need some help here. We need to know what ideas from other insurance contexts apply and what ideas don’t apply.
In some cases, if you get ticketed for speeding or running a red light, it shows up as higher premiums on your car insurance for awhile. Generally, we think that buying life insurance when we are younger rather than older will be less expensive. And if we fail to prune the tall tree near our home and it falls onto our roof, causing us to file a claim–some increase in our premium isn’t too surprising. So how do these ideas relate to health care reform? And if they don’t, why not?
Third, the optimistic outcome relating to health care reform and changes for how our country communicates about health is that we all become wiser about how politics relates to health… So we participate in the political process with our vote in elections and our voice in debate… not just in overcrowded town hall meetings but in the online forums available to us through access to our representatives where we ask questions and persist until we have answers… often and not just when something ‘big’ seems to be in the wind.
In short, we need to keep our eye on the ball and the goal, and make sure that those who represent us do the same…
 April 21, 2010
April 21, 2010
Communication and uncertainty go hand-in-hand. Many of our theories in communication focus on uncertainty as a reason to communicate. In these cases, we usually focus on communicating to reduce uncertainy. We talk about how we use cues from others–such as how they dress, the hair style they wear, the way that they gesture, and even how fast or slow they talk and their accent–to decide how much we are like another person. In these ways, we are using nonverbal information to reduce our uncertainty about talking with someone.
In already established relationships, we also experience uncertainty. Relational uncertainty may happen because we don’t know if our friend or family member is being ‘honest’ about whether they think we should take the job, go back to school, or in a million little day-to-day situations–like what to wear, what to eat, or what to do with our free time. We often try to reduce our uncertainty in these sitautions as well by communicating. ‘What do you want to do?’ ‘What are you doing to wear?’ ‘Do you think I should take this job?’ ‘What about the fact that we can’t sell the house right now?’ ‘They didn’t offer me any moving costs–can we afford it?’ So relational uncertainty emerges in a thousand different ways as part of having relationships. And it is a challenge to imagine how to balance the relationship needs and well, live our lives. So what happens when into the mix we introduce illness?
A diagnosis, whether it is terminal or not–as suggested by one of the participants in my last post–may spark the motivation to communicate. The diagnosis might be for a chronic condition such as heart disease, high blood pressure, high cholesterol, diabetes, or even HIV. It might be a broken leg or a sprained neck. Into each and every one of these and possibly thousands of other diagnoses enters uncertainty. “Illness uncertainty” is a big part of the uncertainy. But “relational uncertainty” is introduced into a diagnosis as well. To improve our communication about health, keeping both kinds of uncertainty in mind may help.
A diagnosis often leads us to want to reduce illness uncertainty about such things as ‘what is it,’ ‘what does it mean for my life,’ ‘how long will it last,’ ‘how will we treat it,’ and a host of other questions that may lead us to seek information to reduce our illness uncertainty. Sometimes, there will be no answers as we seek information, and so we have to “manage” our illness uncertainty by knowing that we have done what we could to answer our questions and perhaps by joining support groups online or in other ways putting ourselves in a position to keep up-to-date with any new information. What we don’t often think about is that in some situations, “increasing” our illness uncertainty may offer the most hope. As an emotion, hope let’s us look forward to a future that is a positive one and where we see ourselves able to achieve important goals. When we do not have certain information about our illness, that may provide a path toward hope if we frame it based on such comments as, “the doctor told me, ‘I don’t see any expiration date on you'”,–meaning that there is no answer to a question framed as, ‘how long do I have to live’.
In some of my past research, I have talked about the acute phase following a spinal cord injuury. During this phase, patients and families often are most reassured by communication that increases their uncertainty about the course of the diagnosis. Doctors not knowing whether a patient will walk again is a hopeful thing. At the same time that the patient and family experience hope related to increasing their illness uncertainty, they may experience sadness and fear and anger about a sense of increasing relational uncertainty. This is a case where friends and family may be very supportive in the beginning but seem to be less so over time. Communication may need to be more direct to reveal what is happening. If a friend asks, ‘what can I do for you?’ and the ansswer is always the same–‘nothing’–the friend may quit asking and quit coming around. There are many reasons that we don’t ask for help–and we can discuss those in the coming days–but if we remember that it may increase a friend’s uncertinaty about the relationship if we say ‘nothing’ and we obviously need help. And their lack of helping when we obviously need help may in turn increase our uncertainty about them. And both may contribute to illness uncertainty in negative ways–relating to a lack of tangible and emotional support–perhaps we can stop the spiral and communicate about our health and our relationship in more fruitful ways… not always to reduce uncertainty… but at least in ways to manage it.
 Taking vitamins is the number one way that U.S. citizens ‘complement’ the formal health care they receive. This is a finding that has been consistent for some years and the 2005 Institute of Medicine Report about use of complementary and alternative medicine [ http://www.iom.edu/Reports/2005/Complementary-and-Alternative-Medicine-in-the-United-States.aspx] considers this reality as well.
Taking vitamins is the number one way that U.S. citizens ‘complement’ the formal health care they receive. This is a finding that has been consistent for some years and the 2005 Institute of Medicine Report about use of complementary and alternative medicine [ http://www.iom.edu/Reports/2005/Complementary-and-Alternative-Medicine-in-the-United-States.aspx] considers this reality as well.
Many debates about using vitamins, minerals, and other supplements — including garlic or herbs or cinnamon or ginger — focus on getting us to eat ‘healthy’ rather than depending on vitamins to make up for a diet that may be lacking. Other debates focus on the cost of ‘unproven’ therapies.
Whatever the debate, keeping track of use increases our ability to report use to our doctors. Talking to our doctors about use may make the difference between a therapy working or not. Many prescribed medications have been found to interact with different vitamins and other supplements, spices, and/or herbs. Sometimes, we need more or less of a medication based on use. So keep track and talk about use to avoid harmful effects.
 February 9, 2010
February 9, 2010
I received a ‘smileworthy’ email from my friend and colleague, Ed Maibach, on Monday. He had received word that one of the articles we co-authored had been named to the 50 most read articles in the Sage journal, the American Behavioral Scientist. In fact, the article is #5 on the list, as you can see if you visit http://abs.sagepub.com/reports/mfr1.dtl
The article’s title, “Competencies for the health communication specialist of the 21st century,” gives some idea why it has been one of the most read publications. The importance of this area both theoretically and in application has been widely recognized. This has contributed to a surge in adding health communication classes to undergraduate and graduate programs around the world. And in adding these programss, the debate continues about the focus of education and training.
As I looked back at the lessons learned to develop the article, I realize that many of these competencies are ones that we all need in order to successfully navigate the health information that might only be described as overwhelming in quantity and sometimes questionable in quality. One of the competencies that health communication specialists may choose as a focus focuses on gaining access to and using various electronic databases. As we’ve discussed on this site before, we all need to harness the skills to do this. One of the most important issues remains the ability to identify the sources of these messages in order to consider the validity of their claims.
The emphasis in the article reflects the importance of understanding the role of both media and interpersonal communication on our health habits. To continue the conversation from yesterday, we too often do not seek formal health care because our family or friends don’t support doing so. And we frequently substitute care from our support networks for formal health care. In fact, one of the roles that many faith-based organizations assume relates to providing support to members sruggling with illness or recovering from events that limit their well-being. This may include injuries on the job or the death of a loved one.
Perhaps one of the most surprising and least considered areas of health communication competence relates to impression management. This, too, flows from the knowledge generated from research and practice in interpersonal communication. I reflect on my own hesitation to reveal my failure to behave in ways that I know I should. I want others to form a positive impression of me and to like me. And it carries over into health realms. Besides wanting to present our own best image, we often–with little thought–help others project their own best image. So we may fail to ask our doctor about something we thought we would be talking about in our appointment because we are thinking that to do so might seem to imply that we are ‘criticizing’ our doctor.
Other competencies related to the 21st health communication specialist that we identified more than 15 years ago that all of us will benefit from include media literacy skills associated with understanding gatekeeping relating to content. As discussed in the former post, media stories about medical research likely appear far ahead of therapies to benefit our well-being related to the research findings. Understanding that media seek to give us novel content supports our ability to reflect on the gap between a story and its translation to our care.
So a competent health communicator likely begins with our intention…to understand, to reflect, and to participate in making decisions about our health in informed ways guided by our efforts and experiences.
 January 12, 2010
January 12, 2010
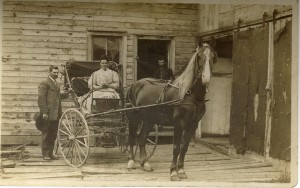
The woman on the horse is a relative that I share a first name with…tho, of course, I never knew her. I wonder what else we might share. Hair color, height, health?
The U.S. Surgeon General advises us to ‘know our family health history.’ The problem is, what to know and how to know it. Since 2004, the Surgeon General has declared Thanksgiving to be National Family History Day [http://www.hhs.gov/familyhistory/] as part of an initiative to get us talking. While we do need to find a time to talk with our family about our health histories, few things seem more doomed to failure than pushing families to talk about poor health at a gathering aimed at celebrating.
First, older adults in our families have many interesting things to tell us about that go on in their lives besides poor health. Many have good health and no reason to focus on poor health. Many want to avoid the stereotype linked to old folks talking about their health and nothing else…even when they do have poor health.
Second, younger adults who need to know about their family health history need to know details that are unlikely to be discussed in such public settings, or if they are discussed, unlikely to be remembered.
Third, it is not particularly helpful to know that there is diabetes or heart disease or cancer in your family if you don’t also know who had the condition, at what age they had the condition, what treatment they used to address the condition, and with what success. Or, knowing what family members have died from should be accompanied by information about the age at time of death.
In this era when we have more awareness of how genes affect health and our reponses to medications and other therapies, we may want to know whether our family members have had any genetic tests. If they have, what ones led to positive results indicating the presence of a particular form of a gene?
Talking about family health history is important but can be difficult if we don’t make time and don’t know what to talk about….